Clinical Services
We offer individual therapy for adults and children as well as couples therapy. All treatment begins with a free initial intake appointment where we meet with you to ensure we are a good match to meet your needs. During your intake session, we’ll ask questions about your symptom history, what is bringing you in for treatment, and what you’d like to achieve during treatment.
Therapy is most useful when you understand your options, know what you are hoping to achieve by engaging in therapy, and have a strong alliance with your therapist. We will support you in creating a plan that aligns with your values and goals while fostering a genuine, empathic, and non-judgmental environment.
Clinical Services at BHIDC
We specialize in evidence-based treatments for adults, children, and couples. If you are seeking support, but don't see a description that fits your concern, please reach out. If we don't specialize in an area that you need support with, we can help you find someone who does.
Anxiety is a normal emotion and common experience, and it represents one of the most basic of human emotions. At one time or another, all of us are likely to feel “stressed out,” worried, fearful in certain situations, and concerned about what other people think. In general, anxiety serves to motivate and protect us from harm or unpleasant consequences.
For many people, however, constant or excessive anxiety disrupts their daily activities and quality of life; for others, panic, which seems to come out of nowhere, can cause terrible physical symptoms, such as faintness, chills, and even extreme chest pains. Anxiety disorders are so common that more than 1 in every 10 Americans will suffer with one at some point in their lives. Fortunately, anxiety disorders can be treated, generally with short-term, effective, and costefficient methods (source: www.abct.org).
Depression is a common psychological problem, experienced by many people at some time during their lives. One member of most families has experienced an episode of depression severe enough to require formal treatment. Depressed mood is costly to individuals and society as a whole, both economically as well as in terms of quality of life.
The primary feature of depression is a sad mood state, which, in its most severe form, is experienced as a feeling of helplessness, hopelessness, and despair. When people experience depressed mood, it is common for them also to experience a decrease in social activities, problems with relationships, and an increase in crying or “a desire to cry even if you cannot get the tears out” (called dry tears depression) (source: www.abct.org).
Everyone experiences stress. Stress can come from anywhere: day-to-day activities, relationships, work, life changes, illness, even from fun events.
Everyone reacts differently to it. Many people don’t even know they are stressed until they begin to experience serious symptoms. Symptoms can be psychological, physical, or both.
Symptoms can include irritability, lack of concentration, worrying, minor headaches, eating too much or too little, not sleeping well, lower back pain, rashes, an upset stomach or ulcers, migraine or tension headaches, high blood pressure, and chest pains, to name a few. Stress can also make physical problems worse, lower your resistance to disease, and affect how well your body responds to sickness and how well you recover from minor setbacks.
Stress affects us all in one way or another. Some people deal well with their stress. Some people have learned to identify their stressors (those things that cause people to feel stress) and deal with them appropriately. Unfortunately, many of us do not deal effectively with the stressors in our lives (source: https://www.abct.org/fact-sheets/stress/).
OCD is understood to involve the frequent experience of obsessions, compulsions, or both. Most people who experience OCD have both obsessions and compulsions. Obsessions are unwanted or distressing thoughts, images, or urges. Compulsions are defined as repetitive behaviors or thoughts (e.g., having a “good” thought to cancel out a “bad” thought) people feel driven to do to reduce distress. Often compulsions are intended to reduce distress related to obsessions (e.g., repetitive washing in response to concerns about germs and disease). While periodic negative thoughts are a common experience for all people, OCD is defined by the related significant distress and life interference that results from these thoughts (source: https://www.abct.org/fact-sheets/obsessive-complusive-disorder/.)
Most people experience stressful events, but when the event is exceptionally stressful it may be called trauma or a traumatic experience. Certain events— such as a home lost in a fire or even a community in the midst of a flood, a terrible injury in a car wreck, or the loss of family members in a plane crash—are traumatic for most people. The threat of serious injury to yourself or loved ones can also be traumatic. What usually makes an experience traumatic is a sense of horror, utter helplessness, serious injury, or the threat of physical injury or death. In some instances, the survivor of trauma may witness a horrifying event rather than being directly injured or threatened with injury (source: https://www.abct.org/fact-sheets/post-traumatic-stress-disorder/).
Though military personnel and veterans can experience the full range of mental health conditions, research suggests they are more likely to be diagnosed with mood and anxiety disorders, including depression, panic, and posttraumatic stress disorder (PTSD), as well as anger-related disorders. Approximately 25% to 50% of military personnel with these mental health conditions first experienced the onset of the condition prior to joining the military. Though mental health conditions, in general, are associated with increased risk for suicidal thoughts and behaviors, among military personnel, depression, PTSD, and alcohol use problems seem to have the strongest relationship with suicide risk. Research also suggests that mental health conditions that are first experienced after joining the military (as compared to conditions first experienced before joining the military) may have a relatively stronger association with suicidal behavior (source: https://www.abct.org/fact-sheets/military-veterans-mental-health/)
We provide services in person and via a secure telehealth platform. Child services include psychotherapy for anxiety, depression, and interpersonal conflict. Most child therapies will include parental involvement. Our therapists will work to help your child change their emotions, thoughts, and behaviors which are causing them distress.
Many children have fears and worries, and may feel sad and hopeless from time to time. Strong fears may appear at different times during development. For example, toddlers are often very distressed about being away from their parents, even if they are safe and cared for. Although fears and worries are typical in children, persistent or extreme forms of fear and sadness could be due to anxiety or depression.
Anxiety: When a child does not outgrow the fears and worries that are typical in young children, or when there are so many fears and worries that they interfere with school, home, or play activities, the child may be diagnosed with an anxiety disorder (source: https://www.cdc.gov/).
Not all children experience child traumatic stress after experiencing a traumatic event, but those who do can recover. With proper support, many children are able to adapt to and overcome such experiences. Mental health professionals trained in evidence-based trauma treatment can help children and families cope with the impact of traumatic events and move toward recovery.
Effective treatments like trauma-focused cognitive behavioral therapies are available. There are a number of evidence-based and promising practices to address child traumatic stress. Each child’s treatment depends on the nature, timing, and amount of exposure to a trauma (source: https://www.samhsa.gov/).
Learn More about processing traumatic experiences with children
Children sometimes argue, are aggressive, or act angry or defiant around adults. A behavior disorder may be diagnosed when these disruptive behaviors are uncommon for the child’s age at the time, persist over time, or are severe. Because disruptive behavior disorders involve acting out and showing unwanted behavior towards others they are sometimes called externalizing disorders (source: www.cdc.gov/childrensmentalhealth).
Body-focused repetitive disorders (BFRD) are when a child causes harm to themself through a habit. This can happen when the behavior occurs often or produces physical and/or mental health problems.
Examples of these disorders include:
- Constant hair pulling
- Skin picking
- Nail biting
- Cheek biting
- Thumb sucking
Most cases of repetitive actions are common, harmless habits and are considered only body-focused repetitive behaviors. Treatment for body-focused repetitive behaviors is only indicated when the behaviors cause significant physical or mental distress for the child (source: effectivechildtherapy.org).
Obsessions are repeated thoughts, urges, or images that cause a lot of worry or distress. Children and adolescents with obsessions may be able to avoid some obsessive worries with effort. Common obsessions include thoughts about uncleanness, safety, doubts, a need to have things in a specific order, or aggressive, sexual, or scary images (e.g., about causing harm).
Compulsions are behaviors or thoughts that a child acts on repeatedly, usually in response to an obsession. Children act on compulsions to reduce distress, or avoid a feared situation or outcome. Common compulsions include hand washing, putting things in order, praying, and asking adults for reassurance (source: https://effectivechildtherapy.org/).
We offer evidence-based couple therapies for relationship distress and couples coping with mental illness. Our clinicians are primarily trained in Integrative Behavioral Couple Therapy, which promotes emotional understanding, improves communication, and facilitates couples working together to handle the bad times and celebrate the good. Treatment typically involves 4 assessment sessions, two conjoint with both partners as well as individual sessions to understand the relationship from each partner's perspective. If couple therapy is a good fit, couples typically engage in therapy for 6-24 months, depending on their needs. At the BHIDC we use the term couple broadly to mean romantic relationships comprised of two individuals who view one another as life partners and have chosen to enter into a long-term committed relationship with one another.
Couple-based therapy for the treatment of depression, OCD, or PTSD
CBT for ADHD
This 8-week group takes a structured, goal-oriented approach to help participants develop and practice skills to manage ADHD symptoms and improve daily functioning.
Details:
- When: Thursdays 6:00 pm to 7:30 pm, September 26 thru Nov 21.
- Where: BHIDC in Ste 3523 Gardner Commons, University of Utah campus
- Cost: $120 for the 8-session group, payable in 2 installments to BHIDC
- Facilitators: Sommer Thorgusen, Ph.D., Libby DesRuisseaux, M.S., & T. Zanooz Cassim, B.S.
- Group Size: Limited to 6-8 individuals for an intimate and supportive environment
- Requirements: Pre-screening with facilitators and consistent attendance encouraged
Pre-screening for new group members is happening now. Learn more here
Caring Connections Grief Processing Groups
We work with the University of Utah College of Nursing who offer Caring Connections support groups for individuals grieving the loss of a family member, friend, or loved one. These 8 week groups are are offered in-person or via telehealth. You can learn more about these groups/check availability by visiting https://nursing.utah.edu/caring-connections or call 801-585-9522.
We offer the following assessment services for Adults:
- Diagnosis of Mental Health Problems
- Personality Assessment
- Attention/Concentration Problems
- Learning/Academic Difficulties
- Intellectual Functioning
- Dementia Screening
- Autism Spectrum Disorders
- Neuropsychological Assessment of cognitive and neurological concerns (e.g., brain injury, stroke, cognitive decline)
We offer the following assessment services for for Children and Adolescents ages 7-17:
- Diagnosis of Mental Health Problems
- Emotional & Behavioral Difficulties
- Attention/Concentration Problems
- Learning/Academic Difficulties
- Intellectual Functioning
- Autism Spectrum Disorders
At this time, we are only able to offer assessment services for English-speaking clients. Not all referrals are appropriate for our training center and we may refer elsewhere for specialty services.
Additional details about the process and cost of assessment services can be found here:
If you have questions about the specific assessment services we offer, please call (801) 581-4697 (Monday-Friday (excluding Wednesdays) 9am-3pm).
Medication management at BHIDC is overseen by Dr. Liz Greene, DNP. Dr. Greene works with each client in a holistic and collaborative way to help restore feelings of well-being and stability. She offers individualized treatment plans by way of comprehensive psychiatric evaluations and ongoing medication management.
If you are interested in receiving medication management through BHIDC, you will meet with our psychiatric provider for an initial 60-90 minute psychiatric evaluation where we will discuss the concerns that brought you in to treatment as well as any pertinent history. At the end of this appointment, we will discuss potential treatment options which may include medication. After the initial evaluation, we’ll typically meet for 15-30 minute medication management follow-up appointments. The frequency of these visits varies depending on the severity of your symptoms, if any changes are made to your medications, and your treatment response. You can typically expect to be seen every 1-4 weeks initially, and then potentially less frequent as determined with your provider.
Please note, BHIDC does not prescribe controlled substances. This includes but is not limited to stimulant medications (ex. Adderall, Ritalin), benzodiazepines (ex. Xanax, Klonopin), sedative/hypnotics (ex. Ambien) or opioid pain medications (ex. Lortab, Percocet). If you are on a controlled substance, you will be referred back to the prescriber of that medication for any refills.
A Research & Training Center
BHIDC is committed to providing high-quality evidence-based treatment to all. Our clinic is a research and training clinic, which means we’ll be asking you to fill out some questionnaires before, during and after treatment. This allows us to make sure the treatments we’re providing you with are effective and helping you meet your goals. BHIDC is staffed by University of Utah faculty who are licensed psychologists and social workers as well as University of Utah graduate level trainees in social work, psychology, psychiatry, and nursing. All trainees are supervised by licensed clinicians who are established in their clinical specialty.

BHIDC does not accept insurance at this time. All services are private pay (out of network). We use a sliding scale model based on your household income and the training level of your clinician. Fees can range from $20 to $140 per session. Depending on availability, you can request the licensure level of your clinician (i.e., masters student, doctoral student, or licensed clinician). Treatment begins with a 90-minute intake appointment free of charge. As part of your intake, we will discuss cost constraints and clinician preferences and after your intake appointment, we will match you with a clinician to fit your needs.
Note: The cost for psychological assessments are different from those listed above. You can learn more by clicking the button below.
LEARN MORE: PSYCHOLOGICAL ASSESSMENTS
Good Faith Estimate Notice
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost.
Under the law, healthcare providers must give patients who don’t have insurance or who are not using insurance an estimate of the bill for medical items and services.
-
- You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment and hospital fees.
- Make sure your healthcare provider gives you a Good Faith Estimate in writing at least one business day before your medical service or item. You can also ask your healthcare provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
- If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
- Make sure to save a copy or picture of your Good Faith Estimate.
Following your free intake, you will receive a Good Faith Estimate for your estimated treatment cost before you begin therapy. Follow this link to learn more about the No Surprises Act.
If you have questions about our fees, please contact our office at BHIDC@utah.edu. While we don’t take insurance, we can also discuss options to submit your therapy bills to your insurance company for reimbursement, though cannot guarantee reimbursement.
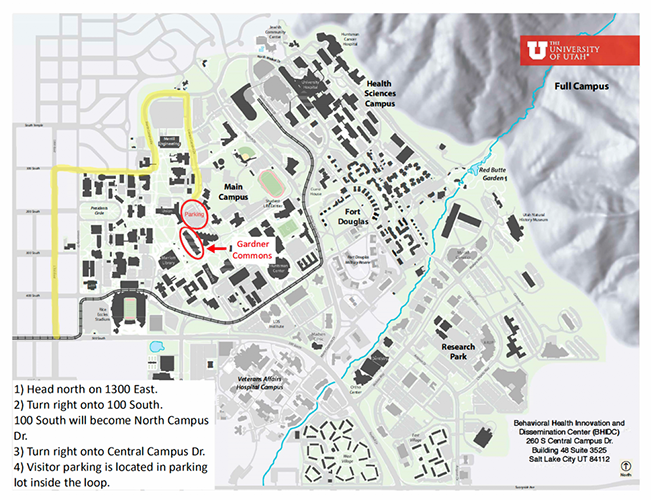
BHIDC is located on the third floor, Suite 3525 of the Gardner Commons Building on the University of Utah Campus, next to the student union. Visitor parking is available in the student union parking lot. If you are a clinic patient, we will provide you with a complimentary parking code. Otherwise, parking is $2.00 per hour.
Gardner Commons - Suite 3525
260 S. Central Campus Drive
Salt Lake City, UT 84112
Need Help Now?
Call the Utah Crisis Line at 988 or 801-587-3000 (local)
24/7 Free and Confidential Services
Available 24 hours a day, 7 days a week, 365 days a year at no cost to you, their certified crisis workers provide:
- compassionate and non-judgmental emotional support.
- suicide prevention, information, and referrals.
- follow-up services.
- psycho-education about mental health issues.
- education on how to support loved ones with mental health issues.
- therapeutic assistance to individuals in emotional distress or psychiatric crisis.
- coordination and dispatch response to individuals in the community as needed via the Mobile Crisis Outreach Team (MCOT) and/or first responders in coordination with other local mental health authorities.
BHIDC follows the Patient Bill of Rights by:
Keeping you informed of the different treatment options that exist.
Discussing the pros and cons of various treatment options and supporting your understanding of the research evidence associated with each option.
Setting agreed upon treatment goals and an understanding of how those goals will be measured.
Developing a treatment plan that is inline with your values and personal goals.
